
COVID-19 vaccination for booster
Available vaccines include: Location & Time Unify Medical Supply1427 S. Federal BlvdDenver, CO 80219 Thurs, Nov. 39AM-6:30PM
...
Available vaccines include: Location & Time Unify Medical Supply1427 S. Federal BlvdDenver, CO 80219 Thurs, Nov. 39AM-6:30PM
...
Unify Health Medical Supply had the chance to partner with SFTP (Service For The People) to bring food to the
...
Unify HSM Brings Thanksgiving Warmth to Denver Communities Collaborating for Community Support This Thanksgiving, Unify HSM has joined forces with
...
Tại sao Bệ ngồi nâng cao Raised Toilet Seats/Toilet Safety Frame lại là giải pháp hoàn hảo dành cho các
...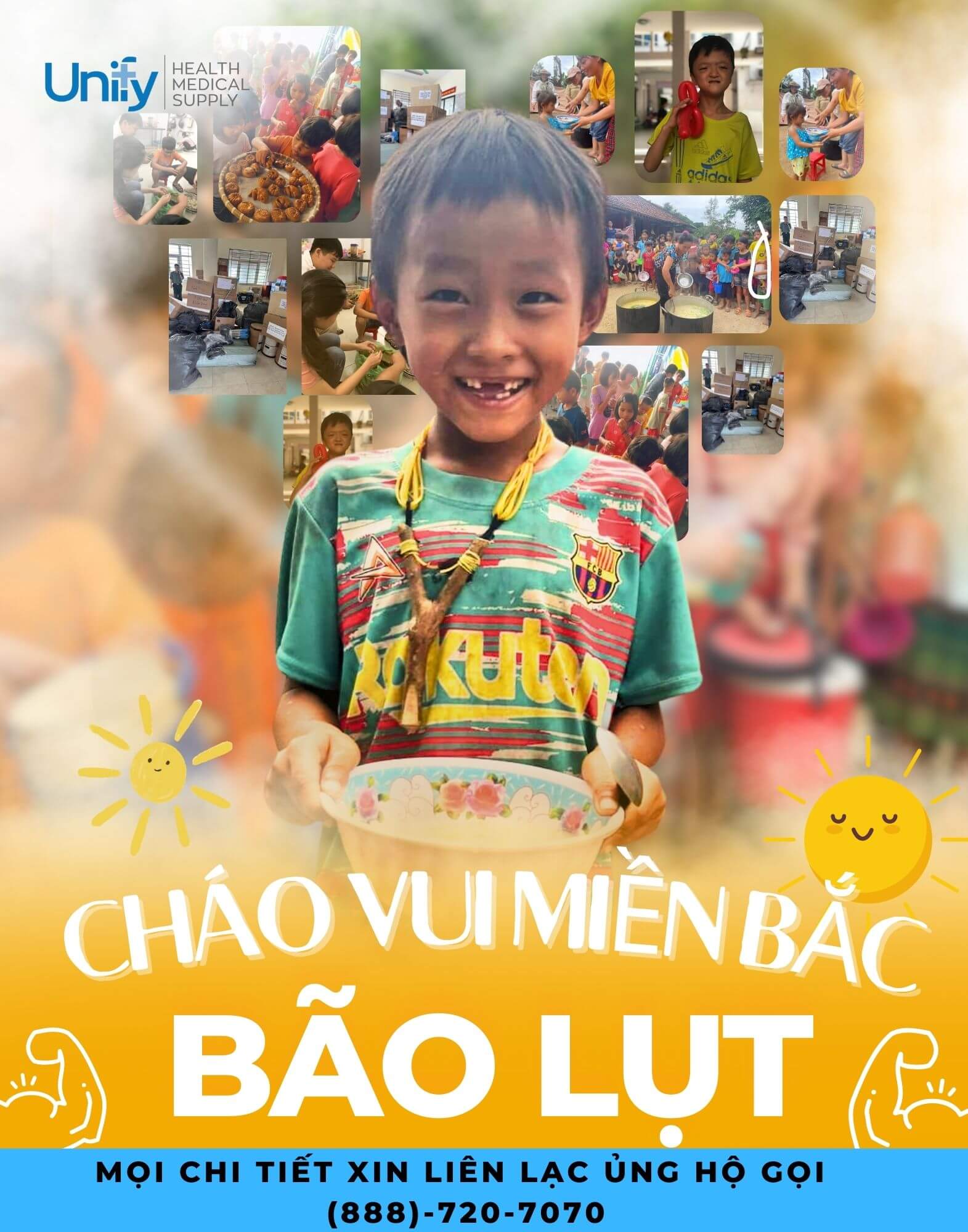
Hậu quả nặng nề của cơn bão Yagi tại miền Bắc Việt Nam Những ngày qua, miền Bắc Việt Nam
...
Trong bài viết dưới đây, Unify sẽ chia sẻ các lợi ích của nhà cung cấp thiết bị y tế
...


Durable medical equipment (DME) and Disposable medical supplies (DMS) are a Health First Colorado (Colorado’s Medicaid Program) benefit that provides clients with medical equipment and/or disposable supplies when there is a medical need for the treatment or therapy of an illness or physical condition.
DME must serve a medical purpose and be able to withstand repeated use. Some examples of equipment that are considered DME include: oxygen, wheelchairs, walkers, and bathroom/bedroom safety equipment.
Similarly, DMS must also serve a medical purpose, but they are not intended for repeated use.
DMS items are items used in active treatment or therapy that are disposable or can be consumed.
Some examples of DMS that are covered include diabetic monitoring supplies, oral enteral formulas and supplies (Ensure, Glucerna, Boost…), and parenteral supplies.
All clients enrolled in Health First Colorado (Medicaid) are eligible to receive this benefit.
The supply of DME/DMS must be prescribed by an appropriate physician, physician assistant, or nurse practitioner and must be medically necessary.
In case you’re not certain about your eligibility, please don’t hesitate to contact our Customer support, we help you with no charge.
Step 1: Your physician will determine the appropriate DME/DMS necessary to meet your medical needs. In some cases, your physician will refer you to a licensed practitioner who will recommend specific equipment.
Step 2: Your physician will write a prescription for the recommended DME/DMS.
Step 3: You may submit the DME/DMS prescription to Unify Health Medical Supply. Unify HMS accepts Health First Colorado. We will process the DME/DMS order and obtain the prior authorization if it is needed.
Please contact our Customer support if you need more information and help!
Yes, we do. DMS such as nutritional supplements (Ensure, Glucerna, Boost,..) and incontinence products (diapers, underpads, gloves, lotion, wipes…) will be provided every month to clients.
Unify HMS can deliver most of our products to clients by one of our company vehicles or through carriers such as UPS®, FedEx®, or USPS. Shipping companies usually deliver in the next business day and, if your equipment is to be delivered by an Unify HMS team member, we’ll give you a date and time window when we’ll arrive.
No, Unify HMS can guarantee it doesn’t cost you anything.
You and your family members will be 100% covered if you are eligible. And your current benefits won’t be affected.
Shipping is free on all orders.
Be sure to check your spam, junk or promotions folder for an email from info@unifymedsupply.com . If you cannot find anything, please give us a call at 888-720-7070
Medicaid requires a prescription in order to cover care products. If you do not have a prescription for you, your Care Specialist will reach out to your doctor directly for the paperwork.
One of our dedicated Care specialists will contact you via phone or email within 1-2 business days of submitting your information. If it has been longer than this time frame, please give us a call at 888-720-7070 and we would be happy to check into your account and provide an update. Our office is open Monday-Friday 9:30 am- 4pm ET.
The number of briefs, pull-ups, and other supplies you receive will depend on what is allowed by your particular state’s Medicaid plan as well as your prescription. Your specialist will let you know exactly the quantity you are eligible to receive.
Incontinence products can be provided for any beneficiaries who have Medicaid as their primary or secondary provider.
You can always adjust the amount of supplies you receive each month.
You can use our online website to easily request fewer items. If you are in need of more items, call us for updating at 888 720 7070